Deep Dry Needling & Chronic Non Specific Neck Pain
Two papers recently just published bring together important information in regards to needling effectiveness and research design.
Paper 1.
The first discusses a long standing issue in the area of complementary and alternative medicine (CAM) e.g. needling research - that being, are we looking at the right method of assessing these interventions by using the gold standard of a double blind randomised controlled trial (RCT). One of the biggest issues relates to blinding the practitioner - pretty difficult when performing a technical procedure like inserting a dry needle! Another issue relates to the importance of the context of the treatment. A RCT aim to isolate and standardized one 'key' factor or ingredient and analyse the effect of this factor against a placebo intervention. Often in CAM, the intervention is personalized and specifically tailored for the individual, putting it at odds with the RCT framework.
Access full text here http://aim.bmj.com/content/early/2016/09/01/acupme...
Paper 2.
Design
The second paper reports probably the most comprehensive study examining the effect of deep dry needling (DDN) in myofascial pain syndrome. The authors used a single blinded RCT design examining deep needling in chronic non specific cervical pain participants.
The authors were at pains (apologies for pun) to point out limitations that had been identified in previous studies and as a result they designed and powered this study to prevent similar mistakes being repeated. In this trial only the therapists knew which group a participant was allocated to, the person carrying out assessments did not and theoretically the participants did not.
Intervention
There was a lot to like about the design and its relevance to clinical practice;
- Intervention group received DDN (n=65) plus stretching and control group received stretching (n=65) only
- 4 treatment sessions were applied over a 2 week period
- They treated all trigger points found in the named muscles
- They treated muscles bilaterally
- Follow-up was for 6 months
Assessment
These were made at baseline, after 2 sessions of intervention, after the intervention period, and 15, 30, 90, and 180 days after the intervention and included;
- Pain intensity (using VAS pain)
- Mechanical hyperalgesia (using analogue algometer over trapezius, levator scapulae, splenius crevicis, multifidi)
- Neck active range of motion (using Cervical Range of Motion goniometer)
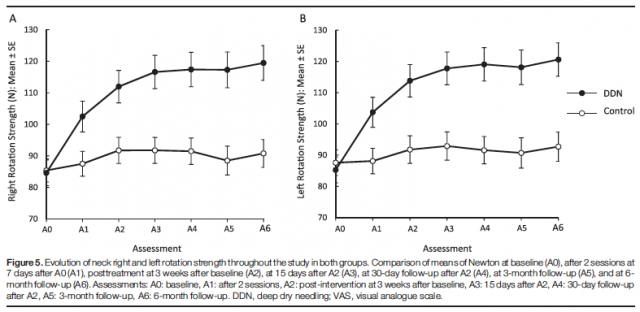
- Neck muscle strength (using MicroFET 2 MT Digital Handheld Dynamometer)
- Perceived neck disability (using NDI)
Safety
Some soreness and local bruising was noted. No adverse effects were reported by participants or observed by therapists.
Results
Significant and clinically relevant differences were found in favor of dry needling in ALL the outcomes measures (all P < 0.001) at both short and long follow-up periods.
Comment
Firstly, I liked the comparison of stretching to stretching plus DDN. Why? Because I have found that when attempting to conduct gentle muscle stretching on upper trapezius or levator scapulae in clients with CNSCP, it feels like trying to stretch rubber (just rebounds on relaxation of the stretch) and usually results in more pain. This was also noted by Edwards et al**.
Secondly, while no strength training was included in the treatment protocol, there was a significant increase in participant's strength, implicating weakness due to pain inhibition due to trigger points. The passive stretching group (control) did not gain in strength.
Clinically I find that there is quicker success when treating clients with myofascial pain syndrome in the cervical spine cf. lumbar spine. I reason that this is generally load related; being there is a greater load in the lumbar spine resulting in more situations that involve a chemical process overlay on top of the myofascial pain syndrome (mechanical process). Speaking of overlay, I also find there is more psychological overlay when you have a 'back' problem cf. a 'neck' problem and for this reason discuss lumbar pain in terms of 'just like spraining your ankle', to which people seem to have no emotional baggage.
Fantastic paper from this research group in Madrid, Spain. Abstract can be found here:http://journals.lww.com/pain/Citation/2016/09000/Effectiveness_of_dry_needling_for_chronic.7.aspx
**Edwards J, Knowles N. 2003 Superficial dry needling and active stretching in the treatment of myofascial pain: a randomised controlled trial. Acupuncture in Medicine 21:80–6.
Subscribe for your 19 Gems of Dry Needling Wisdom

Wisdom Series: 19 Dry Needling Emails
**What Are Trigger Points**
**Grading & Recording**
**Clinical Articles**
**Latent Trigger Points**
**Needling Techniques**
19 emails in 20 weeks. Receive your weekly inspiration of green clinical tea!